It’s true that PCOS and pregnancy aren’t exactly the best of friends.
Affecting how often you ovulate, PCOS can make it more of a challenge for sperm and egg to have that magical meeting.
But getting pregnant with PCOS is by no means impossible – quite the opposite, in fact.
A small word of warning: if you’re after a tell-all guide on exactly how to cure PCOS naturally and get pregnant, we’re sorry to say that such a guide doesn’t exist.
What works for one mama may not work for you, and vice versa.
No PCOS journey is the same, but the community is bigger than you think, and every insight has value.
So we reached out to embryologist and fertility expert, Navya Muralidhar and the PCOS community on Peanut for tips and tidbits to try to increase your chances of getting pregnant with PCOS.
In this article: 📝
- What is PCOS?
- How do you get diagnosed with PCOS?
- Can I get pregnant with PCOS and on birth control?
- What are the chances of getting pregnant with PCOS?
- Why is pregnancy difficult with PCOS?
- Can I get pregnant with PCOS naturally?
- How do you know when you’re ovulating with PCOS?
- How can I increase my fertility with PCOS?
- Does getting pregnant with PCOS have any risks?
- What are PCOS pregnancy symptoms?
- Does PCOS disappear after pregnancy?
What is PCOS?
PCOS (polycystic ovary syndrome) is an endocrine condition that affects about 7% of women across the world and around 5 million women in the US alone.
It’s one of the most common endocrine disorders in women.
(Endocrine refers to the glands and organs that make hormones.)
According to the Department of Health & Human Services, as many as one in ten women in their reproductive years have PCOS.
And some research suggests that the true numbers are even higher.
And while the effects of PCOS are long term (it’s been linked to type 2 diabetes and cardiovascular risks), it’s best known as the most common cause of infertility.
This is largely down to the hormones (aka the chemical messengers in your body) being totally out of balance with androgen levels on high and ovulation turned down low.
Common symptoms of PCOS include
- Irregular periods (or a lack of periods, known as amenorrhea)
- Weight gain
- Acne
- Facial hair or extra hair on other parts of your body
- Hair loss
- Mood swings
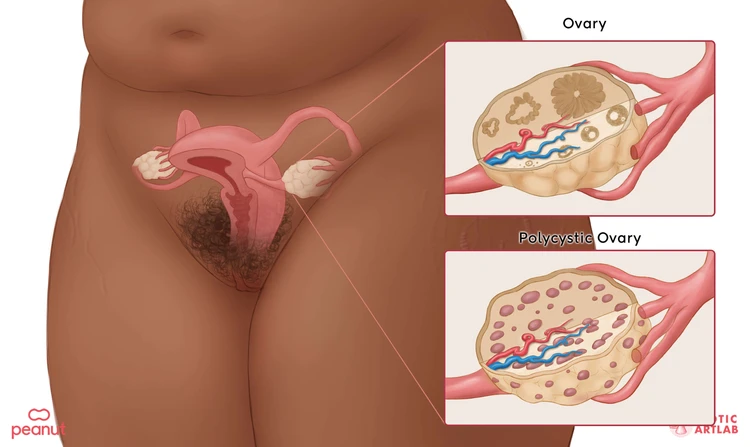
- Lots of (harmless) fluid-filled sacs in your ovaries (hence, polycystic ovary syndrome)
- Hyperglycemia (sugar rush)
- Depression and anxiety
- Enlarged ovaries
- Skin tags, which are small growths of excess skin, often on the neck or armpits
- Dark skin patches on your neck, breasts, or armpits (known as acanthosis nigricans)
As for what causes PCOS? The jury is still out on that one.
Some studies suggest that people are born with PCOS, implying it’s genetic (or luck of the draw), and others put forward that it can be caused by lifestyle choices.
Many women aren’t even aware of symptoms at all and only get diagnosed with PCOS once they start trying for a baby.
Some women have already had a baby.
What we do know is that there are ways to alleviate your PCOS symptoms, and these tend to vary from woman to woman.
How do you get diagnosed with PCOS?
Your doctor will check for PCOS by doing a full history and physical exam.
They may also do a pelvic exam to see if your ovaries are enlarged.
Blood tests to check your hormone levels are also a helpful diagnostic tool, as are ultrasounds which can look at your ovaries in more detail.
The diagnosis is made based on the Rotterdam criteria, meaning you need to have two of these three symptoms):
- Oligoovulation/anovulation
- Hyperandrogenism
- Polycystic kidneys
If you have PCOS, you’re also more likely to develop the following conditions:
- Type 2 diabetes
- Infertility
- Hypercholesterolemia (high cholesterol)
- Hyperprolactinemia (higher normal levels that prolactin, the hormone responsible for breast milk production)
- Heart problems
- Non-alcoholic fatty liver disease
- Endometrial cancer
- Sleep apnea
- Depression and anxiety
Head here for our tips for dealing with PCOS.
It can also be tricky to know whether you have PCOS or endometriosis.
Endometriosis is a condition where uterine lining cells grow outside of the uterus.
It can also disrupt your periods and make it harder for you to get pregnant.
But as we talk about in this article, some of the other symptoms and the root causes are different.
(If you’re curious about endometriosis and pregnancy, head here.)
Can I get pregnant with PCOS and on birth control?
Finally, if you’re trying to not get pregnant, you may be wondering if birth control treatment for PCOS is enough to stave off this possibility.
Chances are very low that you’ll get pregnant on combination birth control (that’s the type that they use to treat PCOS).
If used effectively, the pill is 99% effective at preventing pregnancy as long as you take it as instructed.
So if pregnancy is not something you’d like to happen in your immediate future, you’re good to go.
And one of the great things about hormonal birth control is that if, later on, you decide you would actually like to get pregnant, it’s still completely possible!
What are the chances of getting pregnant with PCOS?
There’s no doubt about it, TTC with PCOS is difficult.
But it isn’t impossible.
Peanut is filled with inspiring success stories from women who’ve been where you are:
- “I have PCOS and was also treated for pelvic congestion syndrome. For years I was told that it would be highly unlikely that I would be able to conceive. My partner and I took pre-conception tablets for around six months and started trying. I tried to keep relatively active, healthy, and stress-free, and by my third cycle, I had conceived. We were both gobsmacked that it happened so quickly, and here we are with a little under 7 years to go. Every sufferer is different, and it isn’t always a bad news story.” – Katie
- “Diagnosed with PCOS when I was 18 (12 years ago). Came off the pill last year and cycles all over the place. Thought I would never get pregnant. I used ovulation sticks when I finally got a period (I know they don’t work for everyone with PCOS) and fell pregnant within two months. No matter what your journey ends up being, you will get there!” – Bec
- “I did! It took me almost two years, but I have PCOS, Endometriosis, one tube is blocked, and I have the hormone levels of a woman 10 years older than me! But I have a baby girl who was conceived naturally! – Merissa
For every anxious post asking for guidance or hope, you’ll find endless stories of happy resolutions.
But that’s not to say the road to parenthood is easy or that it looks the same for everyone.
At the end of the day, the chance of pregnancy with PCOS depends greatly on the severity of your PCOS, how long you’ve been trying to conceive, your age, your lifestyle, and your circumstances.
As many Peanut women will affirm time and time again, no sufferer is the same – but it doesn’t mean you’re alone.
Why is pregnancy difficult with PCOS?
Before we delve into why getting pregnant with PCOS is so hard, we want to remind you that none of it is on you.
One of the most frustrating parts of PCOS is how long it takes for a PCOS diagnosis.
Between the hormonal condition presenting in such a wide variety of ways and doctors knowing very little about why it happens, getting diagnosed is half the battle.
On average, it takes two years for a diagnosis and sometimes multiple doctors.
All this to say, carrying shame, guilt, or responsibility is an unnecessary energy when the road to TTC success is already an uphill battle.
Be easy on yourself. 💛
As for why getting pregnant with PCOS is so hard?
One word: ovulation.
Your ovaries releasing an egg is key to getting pregnant, and without that, any friendly sperm that turn up are going to be disappointed.
Usually, ovulation takes place about once a month, but when you have PCOS, it might be a lot more unpredictable than that.
This could be because your hormones aren’t directing your ovaries to release an egg or because the extra sacs (or cysts) in your ovaries are getting in the way of an egg being sent out.
With ovulation being a bit on the random side, it’s quite hard to schedule sex for that promising meeting between egg and sperm.
Meaning trying to conceive with PCOS can take a little extra work.
But again, not impossible.
Can I get pregnant with PCOS naturally?
Getting pregnant with PCOS naturally (that is, without medical treatment) is entirely possible.
In fact, the majority of women conceiving with PCOS will give birth at least once in their lifetime, without any fertility treatment.
Depending on which symptoms of PCOS you’re experiencing, you may also be able to make certain lifestyle changes that can boost your chances of conceiving.
For example, PCOS is often (though not always) associated with weight gain, which can make it more difficult for you to get pregnant
The good news is that weight loss of just 5% has been shown to significantly improve the symptoms of PCOS.
So, if you think losing weight might help you tackle PCOS and smooth the way to pregnancy, you can chat with your doctor about the best ways to achieve this.
A couple of good tips to get you started include:
- Eating a healthy, balanced diet with plenty of fruit and veggies, whole grains, and lean protein. If possible, avoid processed foods that are high in fat or sugar.
- Making time to exercise by walking, jogging, swimming, or taking part in any other fun fitness activities.
Don’t worry – we’re not talking about running marathons here!
One scientific study showed that brisk walking combined with a healthy diet helped women with PCOS improve their menstrual cycle regularity by 50%, increasing their chances of getting pregnant with PCOS naturally.
Small steps can still be really effective.
And we have a whole list of tips from PCOS nutritionist Tallene Hacatoryan to get you there stress-free and at ease.
How do you know when you’re ovulating with PCOS?
If you have PCOS with regular periods, there are a few key ovulation symptoms to look out for:
- Increase in cervical mucus (discharge).
- Your cervix feels higher and softer
- You’re feeling more… in the mood
- You feel something like period cramps, but no period.
- Your breasts feel tender
- You have a headache and/or nausea
- You notice some bloating
Your basal body temperature also raises a little directly after ovulating, which, if you’re tracking it for a few cycles, can help tell you when you think you might be ovulating next, and when is best to be more actively trying to conceive with PCOS.
If your ovulation symptoms are all over the place (which is pretty common with PCOS), then you can always try an ovulation test.
Just keep in mind these are less accurate for people who are TTC with PCOS, so it’s worth checking in with your doctor about which is best for you.
How can I increase my fertility with PCOS?
When it comes to PCOS and fertility, we’re sorry to say that there isn’t really a quick fix.
Every pregnancy journey is different, and for you, TTC might be a journey that needs a little push.
If lifestyle changes aren’t cutting it, or if they’re not relevant for you, there are a few PCOS fertility treatment options that your doctor may suggest to speed you along the road to mamahood:
Oral medication
Clomiphene (Clomid) tablets are usually the first treatment to be tried by aspiring mamas with PCOS.
You take them at the start of your menstrual cycle, usually for several cycles, and they encourage your ovaries to release an egg.
A lot of our mamas on Peanut have had success with getting pregnant on Clomid, so if you think it might work for you, pay a visit to your doctor.
There are also a couple of other oral medications that aren’t technically licensed for treating PCOS, but they can be used “off-label” for this purpose.
Like clomiphene, they work to stimulate ovulation.
These are metformin and letrozole.
Metformin is a treatment for type 2 diabetes that helps to balance insulin levels in the body, which is especially helpful for a person with PCOS struggling with insulin resistance.
Other benefits of metformin for PCOS include reducing the risk of pregnancy loss and gestational diabetes.
Letrozole, on the other hand, is a treatment for breast cancer, but it can also be very effective at getting that all-important egg to the right place at the right time.
Injection
If oral medications aren’t working for you, you may be offered an injection of one of a group of drugs called gonadotropins, which include FSH, LH, and hCG.
This is a hormonal treatment that is very good at encouraging your ovaries into action.
One downside is that it can be too effective at stimulating your ovaries, leading to a risk of OHSS (ovarian hyperstimulation syndrome).
Symptoms of OHSS include rapid weight gain, bloating, abdominal pain, and nausea.
Let your healthcare provider know straight away if you experience any of these.
IVF or IVM
When medications alone aren’t effective, the next step is to try a fertility procedure such as IVF or IVM.
IVF (in vitro fertilization) is a procedure where fertility drugs are used to encourage your ovaries to produce some mature eggs, and they are then removed via a technique called “egg retrieval.”
The eggs are placed in Petri dishes with a lab-processed semen sample which contains a higher concentration of motile sperm (your partner’s or a donor’s).
After the eggs have been fertilized and had a few days to grow, one or two of them are inserted into your uterus.
The hope is that they will then snuggle into the uterine lining, and you’ll be on your way to becoming a mama!
Alternatively, your doctor may suggest IVM (in vitro maturation), where your eggs are removed when they’re still immature and then matured in the lab before being fertilized and placed in your uterus.
IVM is often the recommended course of treatment because people with PCOS are at an increased risk of OHSS.
To prevent the same, IVM can be done with little to no stimulation.
The immature eggs are retrieved and matured in the lab using maturation media.
And for these eggs, a procedure called Intra Cytoplasmic Sperm Injection (ICSI) is often done.
Lifestyle interventions
Medication is not the only option when it comes to PCOS treatment.
Lifestyle interventions, especially diet, and exercise, have proven to have an effect on reducing all sorts of PCOS symptoms.
Following a regular exercise regime and low-glycemic-index diet has been shown to really improve the condition of PCOS sufferers, as have, for some people with PCOS, semaglutides, like Ozempic.
(Again, it’s essential to navigate this with your healthcare practitioner.
We all have different health needs and body types, and it’s important that you get the treatment that’s right for you and your unique body.)
The expert guidelines are to get at least 150 minutes of physical activity a week.
This has been shown to improve all sorts of things related to PCOS, including insulin resistance, mental health outcomes, and overall fitness.
Talk to your doctor about what might be right for you and your specific set of symptoms and circumstances.
Our advice?
Do something you enjoy.
Take a walk in nature, dance in your living room, swim, or play a sport you love.
Exercise doesn’t have to be a chore — it can become a part of your week that you really look forward to.
Recent research into a more holistic approach towards PCOS includes psychological and sleep interventions, as well as complementary medicines.
PCOS has a number of overlapping effects on your well-being.
PCOS, as well as struggling to get pregnant, can put a major strain on your mental health.
So an all-hands-on-deck approach may be optimal when it comes to prioritizing your health.
One thing that can really help navigate the challenges that come with this health condition is support.
(That’s why we have a dedicated support group just for this purpose.)
Know that you don’t have to navigate this alone.
There are so many others who are traveling this road with you.
Surgery
If all other options for managing PCOS have been exhausted, then a type of surgery, called laparoscopic ovarian drilling can be done to help improve ovulation.
Here, you’ll be put under general anesthetic, and the surgeon will make a few small incisions in your belly.
The goal is to break through the outer surface of your ovary — PCOS sufferers tend to have thick outer layers on their ovaries — to lower the levels of androgens (especially testosterone) the ovaries are overproducing.
While this procedure can be effective, it’s not without risks.
All surgery comes with some risks, including bleeding and infection.
With this particular procedure, there’s also the chance that the ovaries could be permanently damaged, which could lead to early menopause.
Of course, if you’re looking to get pregnant, this can be devastating.
The best thing to do is discuss all your options with your doctor to see what might be best for you.
While PCOS pregnancy success rates are difficult to judge because women’s circumstances and treatments vary so widely, it’s clear that most women with PCOS will be able to have a baby if they wish to, particularly with some form of treatment.
For example, medical research has shown that women treated with clomiphene or gonadotrophins have a 70% chance of a successful pregnancy.
We’ll take that win any day.
Does getting pregnant with PCOS have any risks?
The plain truth is that, unfortunately, PCOS and pregnancy do come with an increased risk of complications.
These include:
- Gestational diabetes
- High blood pressure
- Ectopic pregnancy
- Pre-eclampsia
- Pregnancy loss
You may also be more likely to need a cesarean delivery (C-section) when you give birth.
Can you have a healthy baby with PCOS?
As you navigate your own struggles with PCOS symptoms, it’s natural to wonder how it may impact your baby.
And while we’re not here for fearmongering, we do believe in keeping you informed no matter how difficult the conversation may be.
So, here’s what we know definitively.
Studies show that infants born to women with PCOS have shown poorer perinatal outcomes than women without.
This typically looks like premature births, low Apgar scores (indicating that baby needs immediate medical care or assistance), and increased congenital anomalies.
There is also an increased chance of metabolic disorders and a higher rate of hospitalization in childhood through adolescence.
And while the studies into the generational impact of PCOS are numerous (and at times overwhelming), more research is needed to develop interventions that work.
What experts do know is that outcomes differ depending on which PCOS features the individual has.
More importantly, lifestyle modifications aren’t necessarily preventative, though they can provide adequate support to those who have it.
As scary as all this sounds, there are many women on Peanut with PCOS who have had healthy, happy, thriving babies.
These studies are one part of a very complicated puzzle, so the best advice we can lend is to share your concerns with a medical expert and together find a roadmap that works best for your mind and body.
What are PCOS pregnancy symptoms?
Okay, so when it comes to PCOS and pregnancy, we know things aren’t all that simple.
Knowing you’re pregnant before taking a pregnancy test can be tricky enough, but when you add PCOS into the mix… well, the waters get muddied even more.
It might be that your usual PCOS symptoms are actually early pregnancy symptoms, like:
- Fatigue
- Mood swings
- Bloating
- Tender breasts
- Headache
If you think there’s a chance you could be pregnant with PCOS, the best thing to do is wait about two weeks after you’ve had BMS (baby-making sex), then take a pregnancy test first thing in the morning.
What is a good pregnancy test for PCOS?
Looking for a good PCOS pregnancy test?
Well, you may be hunting for quite a while ‒ PCOS and pregnancy tests don’t exactly get along.
Because your hormone levels are already high or fluctuating without pregnancy, determining whether you’re actually pregnant with a pregnancy test can be tricky.
A lot of our PCOS mamas on Peanut have said they had a few false positives when it came to PCOS and pregnancy tests.
If you think you might be pregnant, the best thing to do is check in with your doctor for the most accurate result.
Does PCOS disappear after pregnancy?
You might have stumbled across an article claiming “Pregnancy cured my PCOS,” but is there any truth in it?
PCOS after pregnancy will likely still be hanging around ‒ pregnancy is not the only thing your body was designed to do, and while the fluctuating hormones after pregnancy may make it look like your PCOS has gone, it’s probably not the case.
Unfortunately, there is no cure for PCOS, it’s all about managing your symptoms in a way that works for you.
Pregnancy is an individual journey, and no route is the same.
Nowhere is that more true than with PCOS.
There’s a lot to digest here, but you don’t have to process it alone.
If you want to hear about other mamas’ experiences with PCOS and fertility, the conversations are flowing on Peanut.
The door is open. 💛

